Fenotipos Médicos: Ganan los Cirujanos (Apoyado por la Evidencia)

http://www.bmj.com/cgi/reprint/333/7582/1291


An Intervention to Decrease Catheter-Related Bloodstream Infections in the ICU
Long-term Proton Pump Inhibitor Therapy and Risk of Hip Fracture
Impact of Laparoscopic Resection for Colorectal Cancer on Operative Outcomes and Survival.
Early Endoscopic Intervention Versus Early Conservative Management in Patients With Acute Gallstone Pancreatitis and Biliopancreatic Obstruction: A Randomized Clinical Trial.
Cervical spine fracture patterns mandating screening to rule out blunt cerebrovascular injury
Este artículo del New England Journal of Medicine presenta los avances en simulación y otras técnicas para enseñar a los residentes (becados) de cirugía distintas habilidades necesarias para operar
El Centro para Control de Enfermedades (CDC) en conjunto con la Organización Mundial de la Salud (OMS/WHO) ha redefinido a la tuberculosis ampliamente resistente como aquellos Mycobacterium tuberculosis resistente a isoniazida y rifampicina, además de al menos 3 de las 6 drogas de segunda línea: aminoglicosidos, polipeptidos, fluoroquinolonas, tioamidas, cicloserina y ácido paraaminosalicilico.
Meta-analysis of endoscopy and surgery versus surgery alone for common bile duct stones with the gallbladder in situ British Journal of Surgery November 2006 p.1185-1191E. S. J. Clayton, S. Connor, N. Alexakis, E. Leandros
Journal of Critical Care Volume 21, Issue 4 , December 2006, Pages 316-321

Un artículo recientemente publicado en Medicina Intensiva (publicación española) discute aspectos respecto al uso de ADH en el manejo del PCR.
Meta-analysis of preoperative antiseptic bathing in the prevention of surgical site infection British Journal of Surgery November 2006 (p.1335-1341)J. Webster, S. Osborne
Early predictors of prolonged mechanical ventilation in major torso trauma patients who require resuscitation
Use of transabdominal ultrasound to identify intraabdominal adhesions prior to laparoscopy: a prospective blinded study
Streptococcus milleri infections of the pleural space: operative management predominates
The impact of diabetes on outcome in traumatically injured patients: an analysis of the National Trauma Data Bank
Las patologías GES (antes llamados AUGE) son aún y probablemente seguiran siendo por mucho tiempo fuente de discusión. A continuación el link a la editorial de este mes de la Revista Chilena de Cirugía que trata este tema.
Klebsiella oxytoca as a Causative Organism of Antibiotic-Associated Hemorrhagic Colitis N Engl J Med dec 7 2006
Stage migration caused by D2 dissection with para-aortic lymphadenectomy for gastric cancer from the results of a prospective randomized controlled trial Journal of British Surgery Dec 2006 p.1526-1529
Prospective multicentre evaluation of adverse outcomes following treatment for complicated diverticular disease British Journal of Surgery(p.1503-1513)
Surgical strategies for gastric cancer with synchronous peritoneal carcinomatosis BJS (p.1530-1535)S. Gretschel, R. Siegel, L. Estévez-Schwarz, M. Hünerbein, U. Schneider, P. M. Schlag
Strength of evidence for perioperative use of statins to reduce cardiovascular risk: systematic review of controlled studies
Diagnostic Accuracy of Colorectal Cancer Staging With Whole-Body PET/CT Colonography
Acute Nonspecific Abdominal Pain: A Randomized, Controlled Trial Comparing Early Laparoscopy Versus Clinical Observation.
The Effect of Unrestrained Rear-Seat Passengers on Driver Mortality.
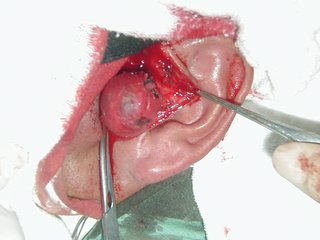
La cirugía endoscópica transluminal (conocida como NOTES por sus siglas en inglés: Natural Orifice Transluminal Endoscopic Surgery) se esta escuchando cada vez más fuerte en la comunidad quirúrgica. Este articulo publicado en Cirugía Española toca este tema del que cada vez aparecerán más trabajos.